Early Childhood Mental Health Toolkit Home > What Works?
What works?
10 Best Practices in Early Childhood Mental Health
Review these top 10 early childhood mental health best practices to consider what fits best with your community’s climate and needs.
1. Screenings for both child and parent are included as essential parts of a child’s developmental assessment. Best practice is to screen for: 1) social emotional wellbeing of the child, 2) pregnancy-related depression and anxiety in the mother and 3) alcohol and drug use in pregnant women.
Why is it a best practice? Screenings can be used to predict risk of a developmental or mental health issue. Because children are frequently in a pediatrician’s office for well-child visits, there is an opportunity to assess the social emotional wellbeing of a child. In addition, post-partum depression or anxiety in mothers can have a significant effect on mothers, children, and families; screening mothers for this during well-child visits is also a best practice in support of early childhood mental health. Screening for alcohol and drug use during pregnancy presents an opportunity to engage women with substance use disorders in treatment and an avenue to prevent fetal alcohol effects and neonatal abstinence syndrome.
If screening results raise concerns, this should be discussed with the family and the child should be referred for further services.
Here are some useful resources and an example of how comprehensive screening is working in Colorado:
The American Academy of Pediatrics’ Bright Futures Guidelines for Health Supervision of Infants, Children, and Adolescents is a seminal resource for health care professionals on pediatric health promotion. It provides a schedule of developmental and mental health items to screen for in infants and toddlers and recommends screening for postnatal depression and anxiety of mothers. Their website includes free resources and materials to support children’s mental health, including screenings.
Colorado’s Assuring Better Child Health and Development (ABCD) initiative works with pediatric health care providers, child care providers, families, and communities to help them identify children who may have potential developmental delays as early as possible. ABCD helps promote guidelines for screenings in primary care settings and works to ensure that once children with potential delays are identified, they are quickly and successfully connected with the assessments and services they need.
Best Practices
Mountainland Pediatrics is an integrated pediatric and behavioral health clinic in Thornton, Colo., that provides child and maternal screenings during well-child visits. Any mother who visits the clinic within a year of giving birth is screened with the Edinburgh Postnatal Depression Scale. If results of the screening indicate that the mother may need additional support, the pediatric provider is able to immediately call in a mental health clinician from the behavioral health clinic. This clinician can complete a risk assessment, and if needed, refer the mother for appropriate maternal care and early childhood services from the behavioral health clinic. The maternal screening can be billed under the child’s Medicaid or as a Z code with the mother’s Medicaid if the child doesn’t yet have Medicaid.
2. Quality improvement strategies for early childhood care and education programs recognize and assess the impact that caregivers have on a children’s social emotional development and mental health.
Why is it a best practice? A quality early care and education environment is one that is designed to intentionally support children’s safety, health, happiness, and learning. The National Association for the Education of Young Children indicates that program quality standards should also evaluate for and support children’s social emotional development.14 As quality is assessed in early care and education, criteria should include items that assess the relationships and caregiving support for children’s mental health.
Here’s an example of how quality improvement strategies in early learning also incorporate mental health:
Licensed early care and education programs go through quality assessment and quality improvement planning. In Colorado, this process is overseen by Colorado Shines, the state’s quality rating and improvement system. Early care and education programs can receive trainings and support from Colorado Shines to improve their quality ratings. Encouraging such quality rating and improvement systems to include specific indicators related to social emotional development, mental health, and quality of caregiver relationships can be an important way to improve overall program quality.
The tools that are used to assess quality of early care and education environment should include ways to assess how caregivers support children’s social emotional development. Early learning programs can review quality ratings tools such as the Infant Toddler Environmental Rating Scale (ITERS-3) and Early Childhood Environmental Rating Scale (ECERS-3) to identify items that integrate social emotional development.
Licensed child care regulations that were added in 2016 also ensure that individuals working with children understand the importance of social emotional development. Under these new regulations, all staff who work with children are required to complete at least three training hours per year in social emotional development. Early learning programs who meet this requirement can receive a higher rating with Colorado Shines.

3. Early childhood mental health consultation is available in early childhood education and home visiting.
Why is it a best practice? Early childhood mental health consultation pairs a mental health professional with the individuals working with young children and their families, such as preschool teachers and home visitors. Early childhood teachers and home visitors are uniquely positioned to influence the environments that contribute to a child’s social emotional and developmental wellbeing. Collaborating with an early childhood mental health consultant further equips these professionals to support children and families. Consultation builds the capacity of the early childhood workforce and is emerging as an evidence-based strategy to support young children’s social emotional development.
You can find practical strategies and resources for implementing early childhood mental health consultation below and an example of how it is working in Colorado:
The Substance Abuse and Mental Health Services Administration (SAMHSA) Center of Excellence for Infant and Early Childhood Mental Health Consultation (IECMHC) helps communities increase their access to evidence-based mental health practices. The Center of Excellence’s IECMHC Toolbox offers interactive planning tools, guides, videos, and other resources to support IECMHC efforts in your state, tribe, or community.
Colorado’s Early Childhood Mental Health Specialist program provides experts in early childhood development and mental health to early learning providers and other caregivers across the state. This is a free resource to support children’s social emotional development from birth through age 8.
Another example is the Play Project, funded by the Colorado Health Foundation and led by the Mental Health Center of Denver (MHCD), which places consultants within early learning centers in the Denver metro area. These consultants are embedded into child care centers to support center directors, staff, children, and families. In addition to embedded consultants, MHCD has two consultants that are on-call for any child care center in Denver County.
“As an Early Childhood Council in rural Colorado, consultants have been a game changer. They help early childhood educators who struggle with children who experience trauma and attachment issues, provide psychoeducation and opportunities for assessments and referrals, and serve as part of warm hand-off systems for families.”
– Early Childhood Council of San Luis Valley

Rural Highlight
Centennial Mental Health Center of Morgan County uses a consultative approach to expand its services to rural and frontier communities. They have increased their number of early childhood mental health consultants for their 10-county region from just one full-time consultant to four, quadrupling their bandwidth of impact.
4. Integrated mental health, substance use, and primary health is covered through public and private health insurance plans.
Why is it a best practice? Increasing numbers of pediatric and primary health care practices have been integrating a mental health provider (e.g., psychologist, licensed clinical social worker, or licensed therapist) into their practice. “Integrated care” is an overhaul of the structure of the practice, so that physical and mental health practitioners not only work alongside one another but team together to systematically coordinate care for patients. Integrated mental health providers can support the use of mental health screenings, provide real-time anticipatory guidance for mental health issues, and respond to mental health emergencies.
Collaboration and shared understanding of roles and responsibilities are key in successful integration of care. Here are some examples of success:
The Colorado State Innovation Model (SIM), funded by the Centers for Medicare and Medicaid Services, is helping practices integrate mental and physical health in primary care settings and test alternative payment models. SIM is supporting four community health centers and 25 percent of primary care providers in Colorado to integrate behavioral and physical health during a four-year period ending in 2019. For early childhood populations, SIM’s focus is on both medical and behavioral preventive counseling and anticipatory guidance. This includes strategies like screening, identification, and referral to early intervention services when risk factors or developmental delays are identified.
SIM has developed practice modules that address issues such as integration of substance use services, adverse childhood experiences, and depression.
Project CLIMB (Consultation Liaison in Mental Health and Behavior) at Children’s Hospital Colorado is another model of successful collaboration between primary care providers and early childhood mental health specialists. Project CLIMB’s integrated behavioral and physical health services allow for comprehensive care that addresses mental health, behavior, and development of children and their families. Integrated behavioral health providers are also able to address caregiver and environmental wellbeing and adversity, helping to identify supports and resources and deliver interventions that allow families with young children to thrive. This program and approach improves access to mental health services and provides young children and families with the full continuum of care–from prevention and health promotion to early identification, intervention, and treatment–while promoting a relationship between the early childhood system of care and primary health care providers.
Healthy Steps is an integrated behavioral health model that supports families with children ages 0 to 3 at various pediatric practices around the state of Colorado. Sites utilize this model to provide families with enhanced primary care experiences. Healthy Steps Specialists work together with primary care teams, meeting with family members during their well-child visit to provide screenings, support, and referrals.

Rural Consideration
Stigma related to mental health services is especially prevalent in rural areas, where there is often a strong culture of self-reliance and mental health needs may not be shared with a provider or professional. Because individuals are living in such a small community, caregivers may not access needed services for themselves or for their children at mental health centers out of the fear that their cars will be recognized by neighbors and friends. Integrated behavioral health services could help to reduce the discomfort associated with accessing mental health care.
5. Caregiver wellness is supported.
Why is it a best practice? The foundations for healthy child development include supportive interactions with all caregivers and a safe environment.
Young children spend significant time with caregiving adults, and these adults have a responsibility to help children develop to their full potential. Interactions between caregivers and young children—especially infants—can impact neural connections in young children’s brains. It’s important for caregivers to consider their own needs, resources, and support systems as well as the needs of the young children in their care.
Issues such as maternal depression, anxiety, or substance use can have lasting consequences on young children’s development if unaddressed.
Here are some ideas for how caregiver wellness can be supported:
The Nurse-Family Partnership is a program that provides first-time parents with support from a nurse who monitors child development and helps parents learn skills for healthy pregnancy and positive parenting. Specially trained nurses in the Nurse-Family Partnership regularly visit young, first-time moms-to-be, starting early in the pregnancy and continuing through the child’s second birthday.
Jefferson County Public Schools Employee Assistance Program (EAP) is available for all staff—including preschool teachers—within the district. The EAP provides free short-term, solution-focused counseling for all of Jefferson County Public School employees. It provides staff with information about counseling resources, maintaining positive mental health, reducing stress, and forming local school Wellness Committees.
Early Learning Ventures gives early learning providers more time to focus on children and families by supporting them in their business operations and quality improvement.
Recently, Early Learning Ventures launched the Teachers, Learning, and Collaborating initiative where monthly teacher learning groups are supported by qualified coaches, trainers, and other professionals. Supporting caregivers includes helping them meet their professional needs, and for early learning and child care providers and administrators, one way this can happen is by freeing up these providers from many of their business tasks and offering learning and networking opportunities. Early Learning Ventures provides support services for business and family to accomplish this.
Health First Colorado (Colorado’s Medicaid Program) provides the Special Connections program for pregnant and postpartum women and their children to access treatment for substance use concerns up to one year postpartum. The Special Connections program provides free screening, counseling, and case management for pregnant women who are enrolled in Medicaid.
Colorado’s Department of Public Health and Environment released an informational brief on pregnancy-related depression and anxiety with a 2020 goal of increasing the number of women who report a health care provider discussed depression during prenatal care to 85.8 percent.

Rural Consideration
More than 13 percent of rural mothers in Colorado experience postpartum depression, which is slightly higher than for other regions.15 Postpartum depression must be addressed to keep mothers healthy and confident in their parenting. Insurance coverage for integrated care across one’s life can help to foster children’s healthy development and caregivers’ wellbeing. Such coverage would be particularly helpful in rural areas with limited access to behavioral and mental health services.
6. Early childhood programs create a trauma-sensitive climate and culture.
Why is it a best practice? Trauma that might occur in a young child’s life can impact how that child develops and functions. These adverse experiences can include unstable living situations, family violence, and parental history of mental health or substance use disorders, and can potentially interfere with a child’s learning, behavior, and emotions. However, young children exposed to these adverse experiences can succeed when supported in environments that are sensitive to trauma. Early childhood care and education settings can provide trauma-sensitive environments that are responsive to the needs of young children who may have experienced traumatic stress.
Here are some resources that are helping communities to become more trauma-responsive:
The Child Trauma Academy is a national not-for-profit organization working to improve the lives of high-risk children through direct service, research, and education. Here you’ll find resources such as videos, e-books, online learning, and photo books that help caregivers such as teachers better understand how trauma impacts children and strategies to support children who are dealing with trauma.
The Kempe Center for the Prevention and Treatment of Child Abuse and Neglect works to improve the care and wellbeing of children by strengthening families, communities, and systems. Kempe’s IMHOFF clinic provides behavioral health treatment to children and families who are dealing with the mental health consequences of difficult life events such as physical abuse, sexual abuse, neglect, or traumatic loss.
Another trauma-informed program, the Mental Health Center of Denver’s Right Start for Infant Mental Health, supports caregivers and young children who have experienced trauma or present behavioral or developmental concerns. Right Start utilizes evidence-based practices to address trauma and behavioral symptoms in children, while also supporting caregivers with strategies such as child-parent psychotherapy, parent-child interaction therapy, case management, and psychoeducation. As a trauma-informed program, all staff—from clinicians to administrative—are educated about trauma symptoms and ensure their interactions with clients are trauma-sensitive.

Rural Highlight
In response to the opioid epidemic, the neonatal taskforce in the San Luis Valley is working with needle exchanges, law enforcement officials, Boards of Cooperative Education Services, and public health nurses to assist addicted caregivers and their newborns.
7. Early care and education settings create environments and conditions that support a child’s mental health, positive behavior, and social emotional learning.
Why is it a best practice? Environments in which children feel safe and can build relationships with trusted individuals have a significant impact on their healthy mental and social emotional development. Early childhood education and care settings should be designed to take these factors into account and be responsive to early child mental health.
Colorado early learning programs have implemented initiatives that create healthy environments supporting social emotional development:
Denver’s Early Childhood Council received LAUNCH Together funding and implemented Conscious Discipline. Conscious Discipline, which implies shifts in practice and philosophy, works best using a grassroots champion approach; one or more persons from an early learning program assist a full-day training to adopt the approach. This person can then begin to talk with others about what was learned and can start using some of the strategies to become the champion of Conscious Discipline.
Bal Swan Children’s Center has become one of the nation’s foremost preschools using the Pyramid Model for Supporting the Social and Emotional Development of Infants and Young Children. Children who attend Bal Swan learn how to identify their feelings, empathize with feelings of others, share emotions appropriately, and problem solve with peers and adults. When children bring these skills home, they impact the way their family interacts with one another.

Rural Consideration
Rural and frontier communities are often “child care deserts,” with relatives, friends, and neighbors providing early care. These informal in-home providers could benefit from learning opportunities that would allow them to gain the specialized knowledge that would improve their support of the social emotional health of the children in their care.
8. An adequate and well-supported workforce is available with specific expertise in infant and early childhood mental health and caregiver engagement.
Why is it a best practice? It’s important for professionals working with young children to have a strong foundational understanding of child development, early childhood issues, and how to engage with other caregivers in a supportive way. Understanding early childhood mental health and using a relationship-based approach at work are not exclusive skills to mental health professionals. These skills benefit all who work with infants and their families. Teachers, pediatricians, occupational therapists, and many others can implement early childhood mental health practices.
Here are some ways that Colorado has worked towards adequacy of the early childhood workforce in early childhood mental health:
Colorado Association for Infant Mental Health (CoAIMH) leads initiatives that support the professional development of Colorado’s early childhood workforce. One initiative they provide is the Endorsement for Culturally Sensitive, Relationship-Focused Practice Promoting Infant Mental Health (IMH-E®), a professional advancement in infant and early childhood mental health. Professionals who have achieved the IMH-E have completed trainings in best practices for supporting early child mental health. The endorsement is a cross-disciplinary indication of competency. Colorado currently has 63 IMH-E professionals across the state.
In addition, CoAIMH provides a course called Colorado Foundations of Infant and Early Childhood Mental Health for Early Childhood Professionals and Partners (Colorado Foundations). This nine-module training is provided locally for infant and early childhood professionals. Through this and other trainings, supervision, consultation, and conferences, CoAIMH is supporting the professional development of Colorado’s early childhood education workforce.

Rural Consideration
Some rural counties lack qualified early childhood mental health specialists in their region. Lack of housing, cost of living, and low pay in rural and frontier communities make it difficult to attract and retain specialists. This shortage can force families, especially those who have children with special needs, to relocate to the Front Range. Telehealth, mobile teams, and developing professional pathways within rural communities can all be important ways to support and sustain early childhood mental health professionals in rural communities.
9. The DC:0-5TM is utilized for diagnosing mental health and developmental disorders in infants, toddlers, and preschoolers.
Why is it a best practice? Infants and toddlers can have mental health and developmental issues that impact their growth. These could include problems that are related to their developmental stage or general problems that show up in young children. If these issues are identified with the appropriate criteria, they can be effectively addressed.
The Diagnostic Classification of Mental Health and Developmental Disorders of Infancy and Early Childhood (DC:0-5TM) was developed by ZERO TO THREE and is a manual specifically for assessing young children under age 6 for mental health and developmental issues. Other commonly used diagnostic manuals do not fully capture relationship-based mental health issues that appear in early childhood, so the DC:0-5TM is crucial for making an accurate diagnosis for young children.
Here’s an example of how the DC:0-5TM can be used as an appropriate tool for young children:
A child psychologist sees a 4-year-old and her parents who were referred by the child’s pediatrician. The psychologist needs a way to assess the quality of the parent-child relationship and the impact of the larger caregiving environment—such as culture, social supports, and psychosocial stressors—on the child’s mental health. Diagnostic tools used for adolescents and adults don’t include a relationship assessment classification between a child and caregivers. However, assessment of these areas will help determine if there is a need for changes or improvements in the parent-child relationship, as this relationship is critical for a child’s development and success. The psychologist uses the DC:0-5TM to determine needed services and create a focus for treatment goals that include the parents.
If you would like to learn more about how other states are using the DC:0-5TM, you can do so here.
Although the DC:0-5TM is the most appropriate manual for understanding early childhood mental health issues, it is not fully recognized by insurance programs in Colorado, which hinders its usage. This is an issue in many states, and so ZERO TO THREE makes four suggestions for incorporating the DC:0-5 into practice:
1) Formally recognize DC:0-5 in public and commercial insurance programs.
2) Develop and share resources that make it possible for providers to use the DC:0-5 for mental health care eligibility determination, treatment planning, and billing purposes. For example, it is possible to pair a diagnosis in the DC:0-5 with a parallel diagnosis in a diagnostic manual that is billable. This strategy is called “crosswalking.” ZERO TO THREE has created a sample crosswalk from the DC:0-5 to the ICD-10.
3) Accept disorders in the DC:0-5 as eligibility criteria for early intervention services (through Part C Early Intervention Services of IDEA).
4) Include DC:0-5 in cross-sector Infant and Early Childhood Mental Health (IECMH) workforce development.
10. Early childhood program suspension and expulsion rates are quantified, and these practices are mitigated.
Why is it a best practice? Disciplinary practices can impact a child’s ability to learn and their experience of safety within early learning environments. Young children who are suspended or expelled are up to 10 times more likely to drop out of high school, experience academic failure, receive disciplinary action later in their academic career, view school negatively, or face incarceration (2014, US Department of Education). The Office for Civil Rights found that suspension and expulsion disciplinary practices for young children disproportionately impact marginalized populations: African American, American Indian/Native Alaskan, English language learners, students with disabilities, and students in special education are more likely to be suspended and expelled.
These highlights can provide examples and help you understand why reducing suspensions and expulsions in early childhood makes sense:
Suspending and expelling young children from early childhood settings can have deep consequences. Early childhood is a time when children are forming the foundation of positive relationships with peers, teachers, and the school institution. If they are suspended or expelled, they are experiencing early education settings as places where they are not welcome or supported.
In 2016, revisions to the Colorado Department of Human Services’ child care center regulations included language to reduce early childhood suspensions and expulsions. Centers must have policies on guidance, positive instruction, supporting positive behavior, and discipline and consequences.
Additionally, centers must have policies in place regarding how decisions are made and what steps are taken prior to suspension or expulsion due to behavioral issues, including steps taken to understand and respond to challenging behavior.
Over the last decade, Denver Public Schools (DPS) has managed to reduce its suspension rate by over two-thirds and expulsion rates by more than 70 percent and is renewing these efforts with a plan to reduce these practices for young children. DPS’ Resolution Towards Ending Suspension and Expulsion of Young Learners re-emphasizes the importance of positive and affirming environments that support students and the negative impact of suspension and expulsion.
The Pyramid Plus Approach, created by the Colorado Center for Social Emotional Competence and Inclusion, provides education and direction on practices in early childhood education that support children’s social emotional development. Strategies in the Pyramid Plus Approach are intended to encourage inclusion and to support young children in building social emotional competencies and reducing the use of punitive practices. The Pyramid Plus Center provides trainings across the state.
Community Assessment Tool: A Checklist
After reading the What works? section of this toolkit, Early Childhood Councils and community advocates can reach out to community collaboratives, early childhood education and child care organizations, and early childhood mental health and other health providers to champion the adoption of best practices in your community, and determine where there are gaps and assess needs. For each of these best practices, determine with your team or among your core leadership (which may vary depending on how you are addressing mental health in your community) which score best matches to your progress in each of the 10 best practices and write this score next to each practice. Then, identify if there is adequate (A), sustainable (S), and dedicated (D) funding to this best practice (if applicable).
16 U.S. Department of Education Office for Civil Rights (March 21, 2014). Civil Rights Data Collection: Data Snapshot (School Discipline).
- We are not implementing this.
- We are not formally implementing this but have some related efforts.
- We have a plan in place to implement this.
- We are implementing this.
- We have policies in place to implement and evaluate this and it is sustainable.
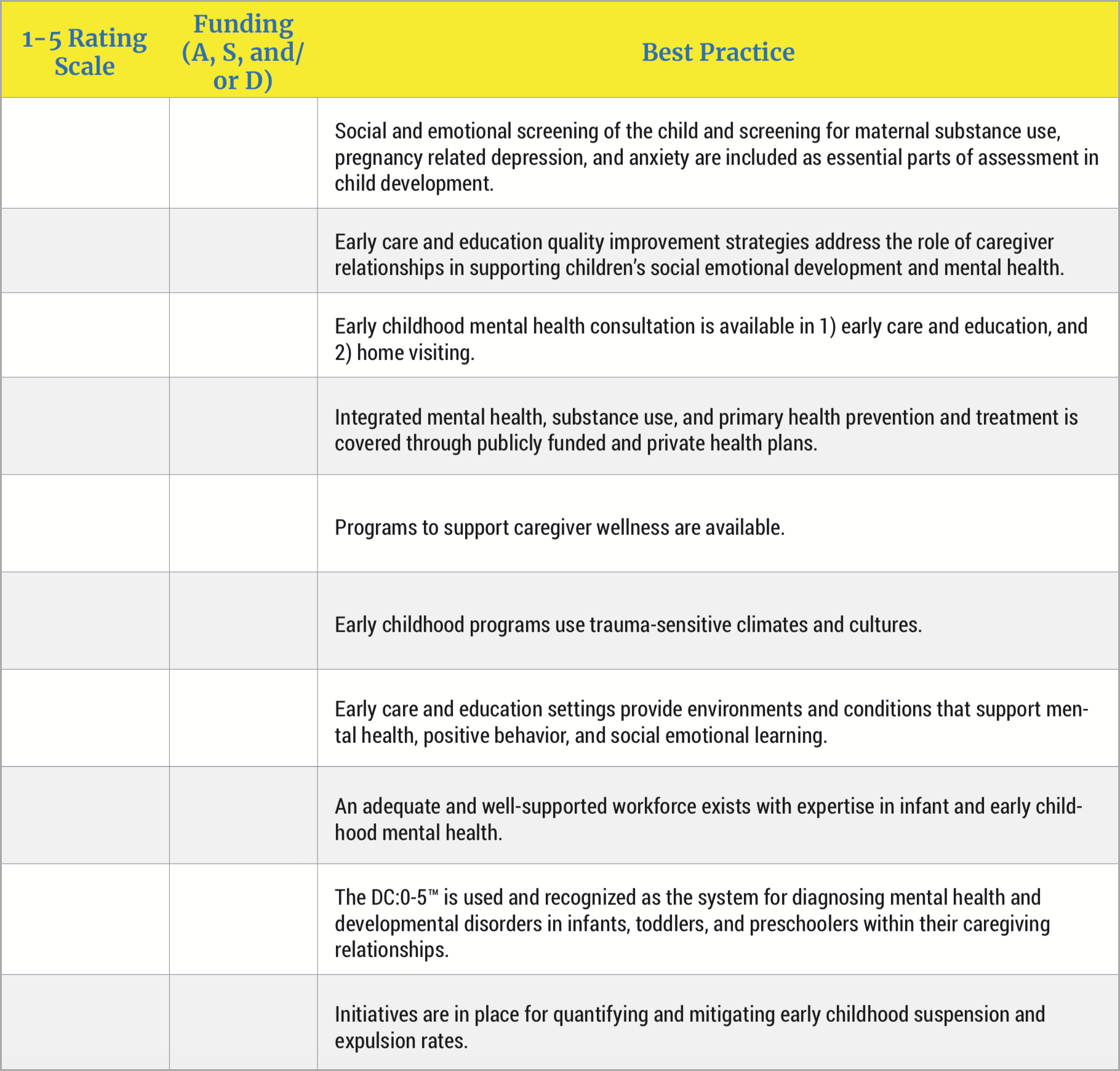
In addition, ask:
- What do you consider the biggest social emotional support or mental health need of children under age 5 in your community?
- What kind of funding needs do you have?
- What does your community need the most help to make infant and early childhood social emotional development a priority?
From here, work with community leaders and champions to develop a brief action plan based on the results of the above assessment; this can focus on priorities for implementing something new or working to sustain what’s already working well.